Your cart is currently empty!
SBO KIT Biotics Research
SBO Kit includes 1 bottle each of A.D.P.®, DYSBIOCIDE®, and FC-CIDAL™ As the understanding of gut microbiota has expanded in recent years, there is now a growing recognition of the extensive influence it has on every system of the body. More than simply contributing to digestion and nutrient metabolism, the microbiota plays an active role […]
Description
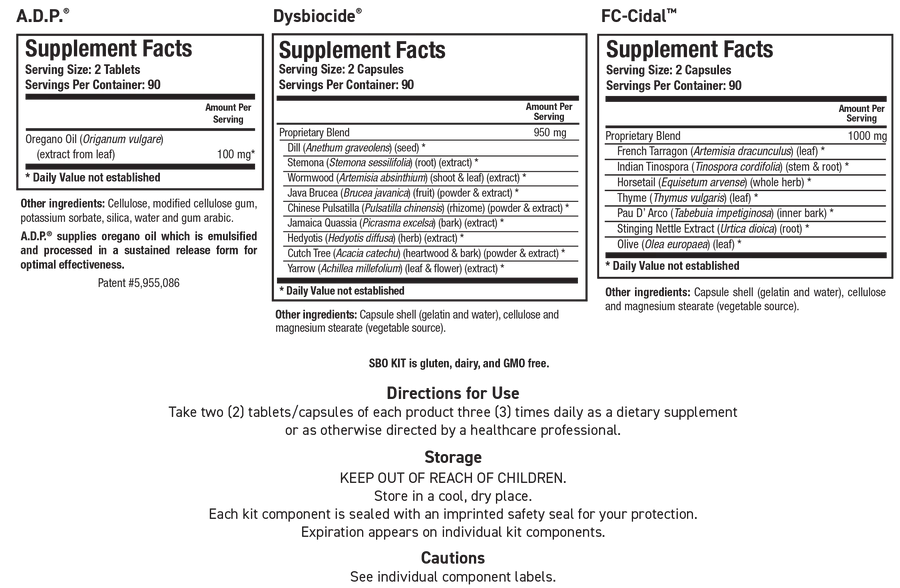
SBO Kit includes 1 bottle each of A.D.P.®, DYSBIOCIDE®, and FC-CIDAL™
As the understanding of gut microbiota has expanded in recent years, there is now a growing recognition of the extensive influence it has on every system of the body. More than simply contributing to digestion and nutrient metabolism, the microbiota plays an active role in cardiometabolic health and function through a variety of mechanisms, including bile acid metabolism and short-chain fatty acid (SCFA) synthesis.
It influences systemic immune function and tolerance, and communicates with the central nervous system via the “gut-brain axis.” In a healthy individual, the gut microbiota performs essential tasks and is a partner in a mutually beneficial relationship. Yet when there is an imbalance in either the functionality, density, or composition of the microbiota, i.e., dysbiosis, it can be a driver for a broad spectrum of dysfunctions. The close ties established between dysbiosis, intestinal permeability, and systemic inflammation have highlighted pathways that may underlie seemingly disparate disorders, ranging from cardiovascular to gastrointestinal to neurological dysfunctions.
Normally the concentration of bacteria increases along the intestinal tract, from a low of 103 CFU/mL (colony forming unit per milliliter) in the stomach to as high as 1011-1012 CFU/mL in the colon, with the small intestine having an intermediate range of 102 -105 CFU/mL.
At bacterial concentrations exceeding this in the small intestine, the risk for multiple clinical symptoms and conditions escalates. For example, the risk for overgrowth among people with functional dyspepsia (characterized by pain, bloating, nausea, etc., following meals) was found to be 2.8 to 4.3-fold greater than among healthy controls, with a prevalence as high as 53%.8 Indeed the most common symptoms reported as a result of overgrowth include watery diarrhea, bloating, abdominal pain, and distension, with an increased risk for multiple vitamin and mineral deficiencies, including vitamins B12, D, A, and E, and iron and calcium.
The prevalence of overgrowth among people with irritable bowel syndrome (IBS) has been estimated to be nearly 5-fold higher compared to healthy controls (with many overlapping symptoms, and IBS subtypes may be predicted by breath gas analysis), and this prevalence is nearly 10-fold higher among those with inflammatory bowel disease.
Given the close ties between cardiometabolic function and the microbiota, overgrowth in the small intestine could be predicted to have a potential influence on cardiometabolic health. Here, too, the evidence supports a connection; a nearly 4-fold risk for nonalcoholic fatty liver disease (NAFLD) was observed among study participants with bacterial overgrowth in the small intestine.
Analysis of individuals living in Western countries found that among those with obesity, the risk for overgrowth was approximately 3.5- fold greater.14 A systematic review of 14 studies found that among people with diabetes, the prevalence of overgrowth was nearly 40%, a nearly 3-fold risk compared to healthy controls.15 Bacterial overgrowth has also been associated with neurodegenerative diseases, particularly Parkinson’s disease, and has the potential for promoting (or preventing) neurodegeneration via several mechanisms, including the production of inflammatory mediators and disruption of the integrity of the intestinal barrier.
Restoring a Healthy Bacterial Balance The initial approach when overgrowth is suspected should be to identify and address contributing factors, primarily any changes to gut anatomy, secretions, motility or immunity. Risk factors include medications used to inhibit gastric acid (proton pump inhibitors (PPIs) and H2 blockers), antibiotics, and motility-altering drugs (e.g., anticholinergics, prokinetics, and opioids), as well as conditions that may alter gastrointestinal motility, such as diabetes and systemic sclerosis.
Perhaps the most well-studied and often employed approach to reducing the bacterial burden is the medication Rifaximin, a nonsystemic antibiotic. However, between 30-40% of people treated with Rifaximin do not see improvement, and approximately 44% experience a recurrence within 9 months of initial treatment.

Reviews
There are no reviews yet.